By Harshit
FLORIDA, DECEMBER 12 —
A new systematic review from Florida Atlantic University’s Charles E. Schmidt College of Medicine reinforces a long-established but often overlooked fact: alcohol consumption — even at moderate levels — increases the risk of several major cancers. The findings highlight striking disparities in vulnerability across demographic groups and emphasize the need for more targeted prevention strategies.
Alcohol is already recognized as a carcinogen by major U.S. health agencies. Yet drinking remains widespread, and the interplay between frequency, quantity, and individual risk factors has remained poorly understood. This review helps clarify that picture by evaluating 62 studies, involving sample sizes from 80 individuals to nearly 100 million, to assess how drinking patterns influence cancer outcomes nationwide.
How Alcohol Drives Cancer Across the U.S. Population
Published in Cancer Epidemiology, the review found clear and consistent links between alcohol consumption and higher risk of:
- Breast cancer
- Colorectal cancer
- Liver cancer
- Esophageal cancer
- Gastric cancer
- Oral and laryngeal cancers
Alcohol use also worsened outcomes in conditions like alcoholic liver disease, contributing to more advanced liver cancers and reduced survival rates.
“Across 50 studies in our review, higher alcohol consumption consistently raised cancer risk, with risk increasing as intake grows,” said Lea Sacca, Ph.D., senior author and assistant professor of population health.
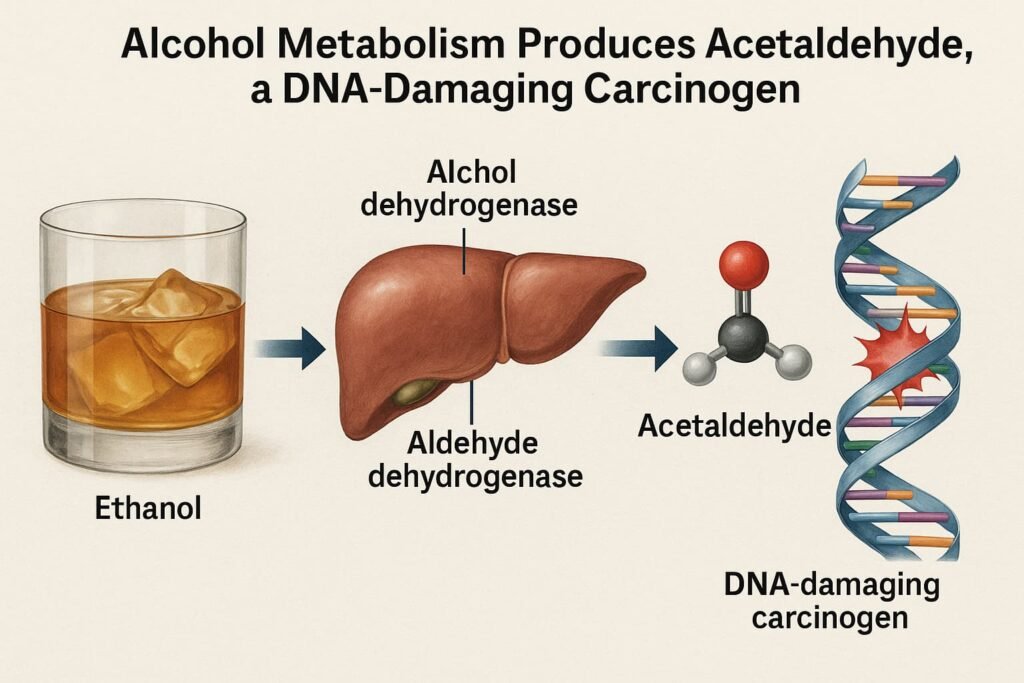
The team documented that cancer risk rises through multiple biological mechanisms, including:
- DNA damage caused by acetaldehyde
- Hormonal disruptions
- Oxidative stress
- Immune suppression
- Increased absorption of environmental carcinogens
These effects compound existing vulnerabilities, making certain groups significantly more susceptible.
Who Is at Highest Risk? Disparities Across Race, Health Status, and Socioeconomics
The review found that risk is not evenly distributed. Alcohol-related cancer risk was substantially higher among:
- African Americans
- Individuals with genetic predispositions
- Those with obesity or diabetes
- Older adults
- Socioeconomically disadvantaged communities
Crucially, some high-risk populations showed elevated cancer burden even when consuming equal or lower amounts of alcohol compared to other groups. Factors such as education, income, chronic disease, and access to preventative care act as risk multipliers.
Individuals who adhered to American Cancer Society alcohol guidelines — or who combined reduced drinking with healthy diet, exercise, and weight control — had dramatically lower cancer incidence and mortality.
Does the Type of Alcohol Matter? Sometimes — And Gender Plays a Role
Across several studies, the researchers observed nuanced differences in cancer risk by beverage type:
- White wine and beer were associated with elevated risks in certain cancers.
- Liquor did not consistently show the same increase.
Gender-based variation was also pronounced:
- In men, frequent drinking was more strongly correlated with cancer risk.
- In women, episodic heavy drinking (binge episodes) showed the strongest association.
Smoking acted as a powerful amplifier of cancer risk in both sexes, though the degree varied by tumor type and drinking level.
Additional aggravating variables included:
- High or low BMI
- UV exposure (melanoma risk)
- Viral infections (HBV, HCV, HPV, HIV)
- H. pylori infection
- Hormone use
- Family cancer history
Even biological characteristics like hair color and eye color emerged as modifiers in some melanoma studies.
Understanding the Biology Behind Alcohol-Driven Cancer
“Biologically, alcohol can damage DNA through acetaldehyde, alter hormone levels, trigger oxidative stress, suppress the immune system, and increase carcinogen absorption,” said Lewis S. Nelson, M.D., co-author and dean at the Schmidt College of Medicine.
These pathways explain why alcohol interacts so strongly with existing metabolic, genetic, and environmental risk factors.
Why Policies Lag Behind the Science
Despite solid evidence, U.S. alcohol policy rarely emphasizes cancer risk. Public awareness remains low, and guidelines vary significantly across states.
The authors call for:
- Stronger alcohol-warning messaging
- Policies acknowledging the social determinants of health
- Targeted outreach for populations with disproportionately high risk
- Integrating alcohol counseling into cancer prevention programs
“Our findings underscore that alcohol-related cancer risk is not driven by alcohol alone, but by a complex interplay of biological, behavioral and social factors,” said Maria Carmenza Mejia, M.D., co-author.
Broader Public Health Implications
With alcohol contributing to at least seven major cancers, and with millions of Americans drinking regularly, understanding these risk dynamics is essential for reducing the national cancer burden.
Effective prevention will require not only encouraging moderation but addressing the environments and pre-existing conditions that magnify alcohol’s harmful effects.