By Harshit, DUBLIN, Oct. 31, 2025
In a major scientific breakthrough, researchers at Trinity College Dublin have discovered that applying mild electrical currents to macrophages—a vital class of immune cells—can reprogram them to reduce inflammation and accelerate tissue repair. The findings, published in Cell Reports Physical Science, could open the door to a new generation of non-invasive, electricity-based treatments for chronic inflammation and wound healing.
Rewiring the Body’s Natural Defenders
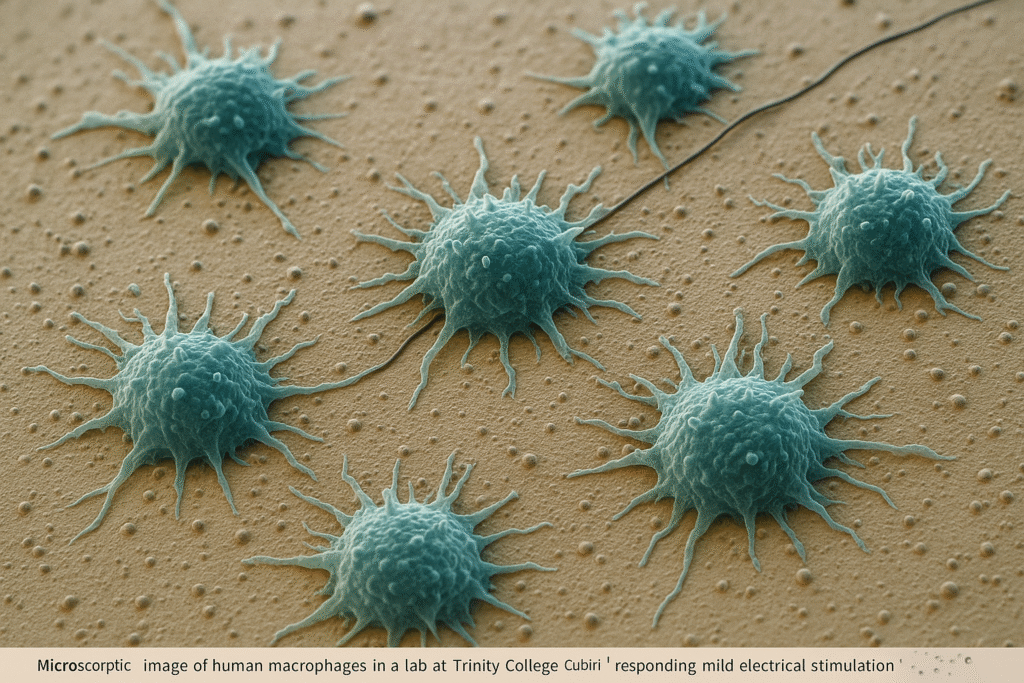
Macrophages are white blood cells that act as the body’s cleanup and defense crew. They patrol tissues, remove dead cells, fight infections, and trigger immune responses when pathogens appear. However, when these cells become overactive, they can release excessive inflammatory signals, leading to tissue damage and chronic diseases such as arthritis, heart disease, and diabetes.
The Trinity team sought to address this problem by exploring how electrical stimulation—a method already known to promote healing in muscle and nerve tissues—might influence the behavior of macrophages.
Testing Electricity’s Effect on the Immune System
The researchers collected macrophages from healthy blood donors through the Irish Blood Transfusion Board at St James’s Hospital, Dublin. Using a custom-built bioreactor, they exposed the immune cells to carefully controlled electrical currents to observe how they would respond at a molecular level.
The results were striking. Electrical stimulation appeared to push the macrophages from a pro-inflammatory (M1) state—associated with tissue damage—to an anti-inflammatory (M2) state that supports tissue regeneration.
According to the study, stimulated macrophages showed:
- Reduced expression of inflammatory signaling genes.
- Increased activity in genes that promote angiogenesis (the growth of new blood vessels).
- Enhanced recruitment of stem cells to damaged tissue, a crucial step in regeneration.
Together, these effects suggest that electricity can “train” immune cells to switch from attacking damaged tissue to actively repairing it.
“Turning Down Inflammation, Turning Up Repair”
Dr. Sinead O’Rourke, Research Fellow at Trinity’s School of Biochemistry and Immunology and first author of the study, highlighted the dual nature of the immune system.
“We’ve long known that macrophages play a central role in both infection control and tissue repair,” O’Rourke said. “But when they overreact, inflammation becomes damaging rather than healing. Our study shows that electrical stimulation can ‘reprogram’ macrophages to calm inflammation and instead promote repair.”
She added that while previous research hinted at electricity’s potential in wound healing, this is the first direct evidence that electrical signals can modify how human macrophages behave.
A Safe, Promising Path for Future Therapies
The research team—led by Professor Aisling Dunne (School of Biochemistry and Immunology) and Professor Michael Monaghan (School of Engineering)—believes the discovery could revolutionize treatment for a variety of inflammatory and degenerative conditions.
Electrical stimulation, they note, is already used clinically in nerve regeneration, muscle rehabilitation, and bone repair, but its application in immunotherapy is new. Because the study used human cells, the results are directly relevant to future medical use, reducing the typical gap between lab research and clinical translation.
“This is the first study showing that electrical stimulation can guide human macrophages to suppress inflammation and enhance repair,” said Professor Dunne. “It’s an exciting step toward using bioelectric therapies to help the body heal itself, rather than relying solely on drugs or invasive procedures.”
What Comes Next
The Trinity team now aims to refine the process by experimenting with different electrical patterns and materials to create more precise and long-lasting effects.
Professor Monaghan explained the next phase:
“We’re developing more advanced regimes of electrical stimulation to fine-tune how inflammatory cells respond. The ultimate goal is to design implantable or wearable devices that can deliver controlled electrical fields to injured or inflamed tissues.”
He added that such approaches could be life-changing for patients with chronic wounds, cardiovascular disease, or autoimmune disorders—conditions where inflammation and poor healing go hand in hand.
Healing With a Spark
The discovery underscores the growing field of bioelectronic medicine, where electricity is used not just to power machines, but to communicate directly with biological systems. By showing that immune cells themselves can be guided by electric currents, the Trinity research marks a milestone in bridging engineering and biology.
As Dr. O’Rourke concluded, “The body already runs on electrical signals—from brain impulses to heartbeats. Our work suggests that, with careful tuning, we can use those same principles to promote healing and restore balance in the immune system.”